Liver and fatigue
Articles are commonplace in the literature outlining fatigue as a concomitant condition with liver pathologies. It is noted especially in any form hepatitis (inflammation of the liver), cirrhosis and fatty liver, regardless of whether the hepatitis is caused by a virus, excess alcohol or fat consumption, or an inherited disease.
Remember, liver disorders have many causes, including autoimmune, heavy alcohol consumption, toxins, drugs, environmental or chemical exposure, viruses or obesity-related liver disease. Fatigue can have both peripheral (i.e., neuromuscular) and central (i.e., resulting from changes in neurotransmission within the brain) causes. Within this presentation, cirrhosis is responsible for 70%‐80% of the directly recorded mortality from alcohol.
Alcoholic liver disease also encompasses a broad spectrum of liver injury, ranging from simple steatosis to alcoholic hepatitis that can be complicated by hepatic fibrosis and
Other conditions such as Haemochromatosis, a hereditary disorder that causes the body to absorb too much iron from the diet, attribute to liver damage along with organ damage through iron deposition. Serum transferrin saturation test measures the amount of iron bound to a protein (transferrin) that carries iron in your blood. Transferrin saturation values greater than 45 percent are considered too high. Serum ferritin test measures the amount of iron stored in your liver. An elevation in Ferritin stores are a good indicator that a HFE test is in order. (2)
Chronic liver disease, regardless of cause or at what stage, is commonly accompanied by alterations in behaviour resulting from disease‐associated changes in neurotransmission within the brain. These changes in behaviour may include fatigue, altered mood (i.e., depression and anxiety), loss of appetite, sleep disturbances and loss of social interest; together these have been termed sickness behaviours. (1)
The syndrome of fatigue is the result of a complex interplay of different factors in different patients. Terminology is also a significant issue with the word “fatigue” often meaning different things to different patients (and clinicians). Peripheral fatigue features can include a reduction in the degree or sustainability of muscle function. Muscle pain can also be prominent. Central features include cognitive abnormalities (such as concentration and memory issues) as well as issues with motivation.
A general consensus is that chronic liver disease (CLD) fatigue is the most common and clinically significant complaint amongst at least 50% of patients. The majority of patients with non-alcoholic fatty liver disease and (up to 70%) and alcoholic liver disease (ALD) (up to 75%) experience significant functional impairment (including fatigue and cognitive difficulties) that affect activities of daily living and which persists over time.
Liver inflammation leads to the production of inflammatory cytokines, including TNF α, IL ‐1β and IL ‐6.
These cytokines can
(a) activate afferent nerve endings (eg. vagal afferents) to induce neural signals that are carried through the spinal cord to the brain, where these signals are relayed within the brain and can alter neurotransmission either directly or indirectly (via microglia activation). Alternatively, cytokines produced within the liver can be released into the circulation;
(b) where they are carried to the brain within the blood circulation. Upon arrival to the brain these circulating cytokines can either enter the brain through areas devoid of an intact blood‐brain‐barrier (BBB ; eg area postrema) or stimulate cerebral endothelial cells which then release secondary signalling messengers (eg nitric oxide) into the brain, which in turn can activate microglia. Alternatively;
(c) immune cells (eg monocytes) can be activated during liver inflammation and are carried within the circulation to the brain where they can adhere to cerebral endothelial cells and enter the brain parenchyma. Upon arrival in the brain these activated immune cells can release inflammatory mediators (eg TNF α ) which directly, or indirectly via microglia, alter neurotransmission.
Changes in neurotransmission within the brain, especially at the level of the basal ganglia impact neural pathways that are critical for the regulation of motivational and reward behaviour. Disruption in these pathways has been linked to the development of central fatigue.(1)
Investigations of bile transport and blood-bile barrier (BBlB) in mice with induced liver disease produced evidence of breaches of the BBIB with impaired bile secretion. (3)
Bile secretion is one of the major functions of the liver, and it serves two major purposes:
1) the excretion of hepatic metabolites—including bilirubin, cholesterol, drugs, and toxins
2) the facilitation of intestinal absorption of lipids and fat-soluble vitamins
Abnormal tight junctions, as a result of inflammation, mutations, or aberrant signalling mechanisms, interfere with proper cell functioning, with subsequent conditions resulting such as cancer and other abnormalities. (4)
Despite its robust and multi-faceted nature, the gastrointestinal barrier can be breached. Local infections by bacteria and virus, exposure to toxins or physical insults, and a variety of systemic diseases lead to its disruption. Such problems can be mild and readily repaired, or massive and fatal.
Tight junctions merge cell membranes together, to form a strong impenetrable barrier. Tight junctions keep contents of cells, such undigested food in the stomach, where it belongs. Additionally, gap junctions allow for the transport of ions, water and other substances. Gastric epithelial turnover occurs on average, twice in a week, where newly generated cells migrate to the lumen. Epithelial injury can be loss of the cell, or break down of the membrane.
During the epithelial restitution phase, immune cells are recruited to sites of mucosal injury to mediate host defence while also participating in reparative responses in the mucosa.
- Neutrophils. Neutrophils are one of the first responders and are recruited to injured sites within hours of damage
- In addition to having direct binding effects on epithelial cells, neutrophils produce or are involved in the biosynthesis of growth factors, such as VEGF, and of pro-resolution mediators such as lipoxins, resolvins, and protectins.
- In response to damage and after the initial influx of neutrophils, inflammatory monocytes are recruited into the wound bed. In the healthy GI tract, a small population of sub epithelial resident macrophages have been proposed to patrol the barrier and release local paracrine soluble mediators that control mucosal homeostasis.
- Infiltrating monocytes that are recruited into the injured mucosa secrete soluble mediators that mediate protection from pathogens, promote clearance of inflammatory cells, and facilitate resolution of inflammation
- Macrophages phagocytose neutrophils to prevent further release of their proteins, thereby further inhibiting tissue injury.
- Inflammatory monocytes/macrophages have been reported to secrete HGF, TNF-α, IL-1, IL-6, and IL-12 to help in host defence and contribute to wound repair.
- Other immune cells. Several other immune cell types encompassing mast cells, eosinophils, and lymphoid cells play an important role in orchestrating mucosal repair.
- Although excess mast cells in chronic inflammation can negatively impact repair, their presence is important in maintaining mucosal homeostasis and reparative processes. Whereas mast cells release several mediators, histamine and prostaglandin D2 have been shown to influence mucosal repair.
- Studies examining tissues from patients with IBD have suggested a role of regulatory T cells (Tregs) in wound repair.
- Mesenchymal Stem Cells. MSCs secrete growth factors and cytokines, which recruit progenitor cells or endogenous stem cells to the injured site to mediate wound repair.
The Gastro-intestinal epithelium serves as a vital barrier that interfaces the external environment containing bacteria and antigens and internal tissue compartments. Injury resulting in a breach of this barrier has detrimental local and systemic effects. The epithelium has a remarkable capacity to repair wounds. It is orchestrated by a spatial and temporal interplay between pro- and anti-inflammatory molecules that mediate cross talk of wound-associated epithelia, neutrophils, macrophages, stromal cells, and microbiota. An imbalance of these interactions can result in delayed wound repair, which is observed in chronic inflammatory diseases. (5)
Restitution of tight gap junctions and the gastro-intestinal epithelium is the cornerstone of the improvement in digestion, absorption, assimilation and elimination. It is through reparation of the gut interface that we are able to restore equilibrium and homeostasis to ensure the correction of disordered digestion, resolution of small intestinal bacterial overgrowth, or other infections such as Helicobacter Pylori, elimination of unwanted microbes and create a healthy gut microbial community.
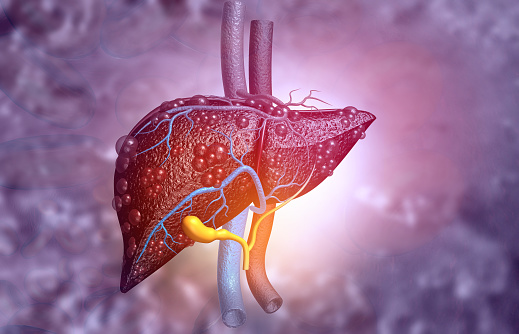
It has been proposed that the liver, the largest internal organ and next to brain in functional complexity, performs a wide variety of metabolic and regulatory functions. Hepatocytes are the structural and functional units of liver and carry out many vital tasks including synthesis, detoxification, and metabolism of carbohydrates, protein, and lipids.
- Tight Junctions are primarily responsible for the barrier properties of the blood-bile barrier (BBlB)
- The hepatic junctions forming BBlB includes tight junctions, adherens junctions, desmosomes, and gap junctions. The tight junction is formed of claudins, occludin, ZOs, and JAMs. Catenins (α-, β-catenin, etc.) and cadherins associate with actin cytoskeleton to form the adherens junction. Gap junctions also provide barrier properties to the liver.
- The BBlB promotes many essential functions in liver including generation and maintenance of hepatocyte polarity and regulation of bile acid secretion and bile flow.
- Loss of BBlB function has been shown to be the primary pathophysiology of cholestasis in children as well as adults.
- Hepatocellular carcinoma (HCC) is currently the worldwide fourth most common cancer in men and the second leading cause of cancer-related death.
- Non-alcoholic Fatty Liver Disease (NAFLD) NAFLD is one of the most common chronic liver diseases characterized by increased fat accumulation in the liver without significant alcohol consumption.
- Liver cirrhosis is a chronic liver injury leading to scarring of liver tissue. A plethora of causes can lead to cirrhosis including alcoholic liver disease, NAFLD, and hepatitis C. or accumulation of bacterial endotoxins.
- Liver Inflammation. The BBlB can also regulate the immune state of the liver or vice versa. Increased intestinal permeability due to the accumulation of toxic bile acids and dysregulated TJs causes an increase in proinflammatory and profibrogenic cytokines including tumour necrosis factor-α (TNF-α), interleukin-1β (IL-1β), and interferon-γ (IFN-γ).
- Specific Probiotic strain administration has been shown to reduce NAFLD in mice. (6)
There has been significant published research into herbal remedies for the liver. The following are several examples that have been researched, but are by no means a comprehensive list.
Remember, it is important to discuss any proposed treatment with a trained health professional to ensure that you are a suitable candidate for any therapeutic treatments.
- Gynostemia -Inhibiting the accumulation of cholesterol and triglycerides as well as preventing oxidative stress by enhancing the production of NO and affects the molecular composition of the mitochondrial phospholipid CL. Reducing the level of serum AST, ALP, insulin, decrease BMI and insulin resistance index.
- Panax NotoGinseng – Attenuating the ethanol induced hepatic lipid accumulation by inhibiting the production of MDA, GSH l and reactive ROS, reducing TNF-alpha and IL-6 levels, as well as enhancing the SOD)activity in liver, and abrogated CYP2E1 induction.
- Dioscin – Relieving oxidative damage, inhibiting inflammation, cholesterol and triglyceride synthesis, decreasing MAPK phosphorylation levels, promoting fatty acid beta-oxidation, and inducing autophagy to improve fatty liver conditions.
- Gallic acid – Recovering impaired glucose and lipid homeostasis in high fat diet-induced NAFLD mice. In vivo Reducing GSSG content and oxidative stress and increasing the levels of GSH peroxidase, glutathione, GSH S-transferase and GSH reductase in liver tissue.
- Baicalin – Decreasing the level of serum total cholesterol, triglycerides, LDL, ALT and AST, and increase the level of serum HDL by mediation of CaMKKbeta/AMPK/ACC pathway. Clinical study-Attenuation of the ischemia/reperfusion injury in alcoholic fatty liver by suppressing of myeloid differentiation factor 88 and TLR4 protein expressions and the nuclear translocation of NF-kB after reperfusion.
- Siliphos – In vitro – Alleviation of the damage of lipid membranes by protecting of mitochondrial function. According to previous studies, the curative effects of Silymarin in alcoholic and non-alcoholic steatohepatitis are widely recognised.
- Berberine – In vitro Reducing TG accumulation in the FFA-induced hepatic steatosis. [81]
- In vivo Enhancing insulin resistance of non-alcoholic fatty liver disease by increasing the expression of IRS-2. Suppression of lipogenesis and promotion of lipolysis by inhibition of the expression of SCD1, FAS, SREBP1c and increasing the expression of CPT1. (7)
- Swain MG, Jones DEJ. Fatigue in chronic liver disease: New insights and therapeutic approaches. Liver International. 2019;39(1):6-19.
- Hereditary hemochromatosis. 09.06.2020.
- Pradhan-Sundd T, Vats R, Russell JO, Singh S, Michael AA, Molina L, et al. Dysregulated Bile Transporters and Impaired Tight Junctions During Chronic Liver Injury in Mice. Gastroenterology. 2018;155(4):1218-32 e24.
- Bhat AA, Uppada S, Achkar IW, Hashem S, Yadav SK, Shanmugakonar M, et al. Tight Junction Proteins and Signaling Pathways in Cancer and Inflammation: A Functional Crosstalk. Frontiers in Physiology. 2019;9(1942).
- Quiros M, Nusrat A. Contribution of Wound-Associated Cells and Mediators in Orchestrating Gastrointestinal Mucosal Wound Repair. Annu Rev Physiol. 2019;81(1):189-209.
- Pradhan-Sundd T, Monga SP. Blood-Bile Barrier: Morphology, Regulation, and Pathophysiology. Gene Expr. 2019;19(2):69-87.
- Hong M, Li S, Tan HY, Wang N, Tsao SW, Feng Y. Current Status of Herbal Medicines in Chronic Liver Disease Therapy: The Biological Effects, Molecular Targets and Future Prospects. Int J Mol Sci. 2015;16(12):28705-45.